Empowering the Employee: Innovations in Healthcare Engagement
Ruben Sigala, Ioan Bolohan, and Marion CouchAbstract: Modern healthcare platform solutions have the potential to transform benefits programs, boost engagement, drive health improvement, and enhance cost-savings / ROI outcomes. Building relevant, bite-sized content that excites members with rewards, personalizing user experiences with machine learning recommendation engines, and applying state-of-the-art consumer marketing practices for lifecycle management can unlock outcomes that significantly outperform traditional approaches.
For years, lack of engagement has plagued healthcare benefits, making them costly, underutilized, and ineffective. Of course, this low engagement is no surprise – navigating benefits is almost impossibly complex. But modern technology may have the solution to unlocking their potential. Combining consumer-grade engagement with a suite of clinically validated content, machine learning-driven interventions, omnichannel accessibility, and advanced data tracking, modern platforms can rewrite how benefits managers reach employees, boost utilization, and drive health improvements. They are game changers.
 Today, most individuals engage with health care professionals for less than 60 mins per year (1). By comparison, they’re on social media for 78,000 minutes per year (2). The solution to short-lived gains, poor access, and episodic utilization is a proactive daily health utility that acts, metaphorically, like an “angel on your shoulder” charged only with the improvement of your whole health and helping you achieve your goals.
Today, most individuals engage with health care professionals for less than 60 mins per year (1). By comparison, they’re on social media for 78,000 minutes per year (2). The solution to short-lived gains, poor access, and episodic utilization is a proactive daily health utility that acts, metaphorically, like an “angel on your shoulder” charged only with the improvement of your whole health and helping you achieve your goals.
In the consumer world, there is an army of people working hard to encourage you to purchase, renew, and subscribe, and another army of people making it easier and easier for you to do so. It is time to apply that same approach to healthcare.
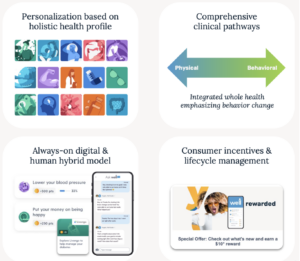
Through a confluence of improved technology, streamlined access via digital devices, and learnings from consumer science, a modern platform can help us be more personalized, persistent, helpful, and rewarding by:
- Using data to personalize interactions based on health history and interests
- Acting as an informed advocate for the patient
- Curating actions to be attainable, rewarded, and persistent
- Customizing incentives to reflect the observed elasticity and importance of each action
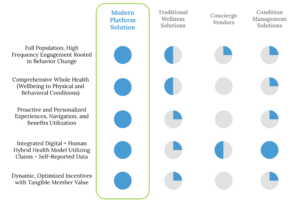
Together, these approaches redefine what a benefits platform can be. They connect the dots across a comprehensive health experience to make engagement meaningful and, importantly, enjoyable for each individual. Ultimately, this modern user experience can improve health, boost employee satisfaction, increase productivity, and generate long-term cost savings and ROI for employers. Envision implementing a program where 80%+ of members report health improvement while driving 10% higher employee retention and 10% direct cost savings (3).
Ask yourself: how engaged are your employees with your benefits offerings today? Are you a consumer-grade solution learning from the top-performing platforms? A world-class program would have utilization rates analogous to those observed among leaders across industries, let alone healthcare. Are 20% of your users active each day? Or 50% active each month? Are 80% of your users “promoters” in your NPS studies (3)? Are you able to drive the engagement and excitement that powers results? This is what modern platforms are capable of delivering. This is why they are game changers. Are you?
State of the Art
Content Library
There is no shortage of health content in our digital healthcare ecosystem, but it holds little value without engagement. To drive sustained, long-term utilization for the broadest possible set of members, content should be designed for mass consumption and reflective of how users engage in a digital environment. It should be varied, comprehensive, multilingual, short-form, and easy to digest. It should draw deeply from behavioral economic concepts to reduce barriers and create continuous opportunities for the member to achieve real-time “wins.” The resulting architecture should revolve around daily, quick, achievable interactions – complemented by multiple pathways, meaningful insights, regular affirmations, and smart incentives to boot. Every aspect intentionally designed to drive ongoing engagement while addressing each user’s health ambitions and priorities to generate buy-in. In short, users have to enjoy engaging with the content.
Imagine translating clinical instructions into a suite of member products that are easy to understand, validated by clinical literature, and targeted with specific unique objectives towards delivering improved health. These range from single health actions to multi-day habit-building journeys, articles, questions of the day, and clinical tracking all aligned with dedicated clinical pathways supporting members’ whole health.
Machine Learning/AI Driven Recommendations Engine
Once a relevant content library is designed to deliver continuous, meaningful engagement with health topics, modern technology, specifically machine learning and artificial intelligence (ML/AI), maximizes utilization. As member engagement generates macro and user-level observations, the AI engine “learns” how to predict the likelihood that a member actually engages with the available content. This “propensity modeling” is continuously refined over time and, combined with the clinical relevance scores of available content, these models prioritize options to surface to the user. Suggestions are then regularly refreshed (alongside randomized, generally applicable content to protect against AI bias), providing members a menu of timely, relevant, and, where appropriate, persistent recommendations to maximize meaningful interactions.
Similarly, these tools can uncover obstacles to engagement. When barriers keep members from engaging in health-promoting behaviors – missing a check-up or skipping a recommended visit – the platform should uncover why. Does a user not trust their doctor? Are they concerned about cost? Do they not have a way to get to their appointment? Or are they simply unaware that they should have visited their provider? Each of these paths requires a different set of interventions to address tactical and perceptual barriers. By systematically revealing inhibitors, the platform proactively personalizes and enhances the user experience. Over time, the predictive capabilities mitigate potential blockers and overcome engagement inertia.
Critically, this data-first approach extends to incentives. Rewards design should borrow heavily from behavioral economic principles geared towards delivering repeat member engagement. While the ultimate goal of improving health takes time – diminishing its efficacy as an intrinsic motivator – platform rewards are instantaneous. The rewards themselves should also resonate with a wide range of members, ensuring that all segments find the prize for their engagement exciting enough to spur a “cue-action-reward” feedback loop.

Member Engagement
Healthcare concerns are often complex, nuanced, and deeply personal. The consumer experience should not all be algorithmically driven. Therefore, platform services should be supplemented by a human frontline supporting clinical, benefits navigation, coaching, and other needs. Bridging the digital and physical divide while providing a trusted advocate to help members navigate their continued healthcare needs. Each exchange with human support should also be captured and fed back into the digital ecosystem for a seamless omnichannel user experience.
In addition, member engagement should be supported by a sophisticated, programmatic, consumer-grade, multi-channel apparatus encompassing everything from evergreen incentive offers to team competitions. Research shows that it can take upwards of 60 touchpoints to generate action (4). This is not the typical approach taken by benefits services. Creating repeat, predictable, reliable interactions and high utilization is a prerequisite for health improvement. This capability has to persist throughout the entire consumer lifecycle, from onboarding to long-term use.
After initiative activation, the ML algorithms should identify key “persuadable” junctures in a member’s lifecycle where intervention can drive engagement. In a digital environment, this means monitoring metrics such as conversion rates, monthly and daily active users, and more – quantifying a pattern of expected engagement for each individual member. From there, automated triggers intervene across multiple channels, delivering persistent messaging and incentives towards ongoing utilization. These should concentrate on members with outsized “lifetime values” and potential for improvement.
Measuring Success

Of course, engagement is only sustainable if users are delighted by their experience. Building member satisfaction is critical to drive engagement. Imagine a war room that correlates tactics with outcomes – testing innovative approaches and continuously analyzing a constellation of carefully curated metrics to generate meaningful and, importantly, actionable insights. “Hero” features, KPI visualizations, and triangulated data from a range of sources all working together to enhance the user experience. With a mobile platform, app store ratings, user chats, and in-app reviews offer gauges of member satisfaction. Supplementing these feedback channels are regular focus groups and surveys reaching the full member population: power users, average members, and non-engagers. Just like the platform seeks to understand why users don’t engage in specific types of content, learning why non-engagers don’t use the platform is key. Again, this is a core difference between a modern approach and the industry status quo. Where the norm is for benefits platforms to offer a uniform service to primarily those who are self-motivated, a modern consumer-first solution aims to be responsive and adapt, catering to the diverse needs of the full member population. Rather than a flat offering that provides transactional or episodic engagement, this approach creates an experience that is inherently enjoyable – transforming daily habits by offering something that actually excites members.
Health Outcomes and ROI
The ultimate aim of all of this is to help all members achieve their best health and drive cost-savings. For health outcomes, picking the right areas of focus is critical and it can vary from one user to the next. With so many data silos – claims, electronic health records, wearables, pharmacy feeds, self-reported health assessments – a world-class solution has to intelligently consolidate sources in a coherent way. Creating a data hierarchy that continuously optimizes the user experience while tracking health improvements.
But bridging these data silos is just the start. It’s not enough for the platform to make strides in advancing member health – the member has to feel progress. Gauging self-perceptions of health status, playing back tracked health metrics, and showing progress – even if in small increments – can go a long way in driving sustained interest and engagement. Furthermore, what a member needs to do to improve their health may be different from what they want to work on. The platform should strive to share knowledge and help put both in reach. This also underscores the importance of having many arrows in the quiver. Platforms must offer multiple ways for members to feel added value from engagement, from follow ups on their goals to celebrations of progress.
Finally, all of this effort culminates in ROI and quality impact. Measuring return goes beyond the traditional approach of calculating savings on chronic conditions. Whole health initiatives largely benefit from lifestyle risk factor reductions, preventive screenings/vaccinations, and utilization management as well as gains from reduced absenteeism, productivity enhancements, and
decreased employee turnover. Mapping condition prevalence reductions and degrees of control to condition costs, utilization measures, and literature on associated benefits offers a proxy for savings realized. These figures can also be cross-referenced with non-activated populations and matched groups in reference datasets to triangulate estimated savings. At employers, sick days, performance ratings, and retention rates combined with FTE and hiring/training costs can similarly offer estimates of value generated by the program. Not to mention savings from eliminating ineffective services and the value of both custom interventions and continuous population-level insights derived from the organization’s own members. Together, these paint a general picture of members who are healthier, happier, lower cost, and more productive.
The Future
So what does all of this look like in the future? Employees gain agency over their health. Users adopt healthy behaviors that are always available, easy to use, and fun. Ultimately, this becomes the cornerstone of value-based primary care delivery models, boosting ROI on wellness benefits. And employers win, too, with engagement driving better recruitment, greater employee satisfaction, productivity gains, cost-savings, and improved retention. This approach enhances health equity without demanding more from already booked up benefits leaders who can depend on their trusted partner to support the member population, helping people make well-informed decisions. Truly a cure for the illnesses that have plagued the benefits space for decades.
Sources:
- Mobius MD, “Are Doctors Spending Less Time with Patients?” Franklin. 2021
- Forbes, “Americans Spent On Average More Than 1300 Hours on Social Media Last Year.” Suciu. 2021
- Well Dot Engagement Reports (2022)
- Tangible Words, “Everything You Need to Know About Touchpoints in Marketing.” 2019.